Health
Archive
764 results
- Task Force Report
U.S. Economic Security
![]()
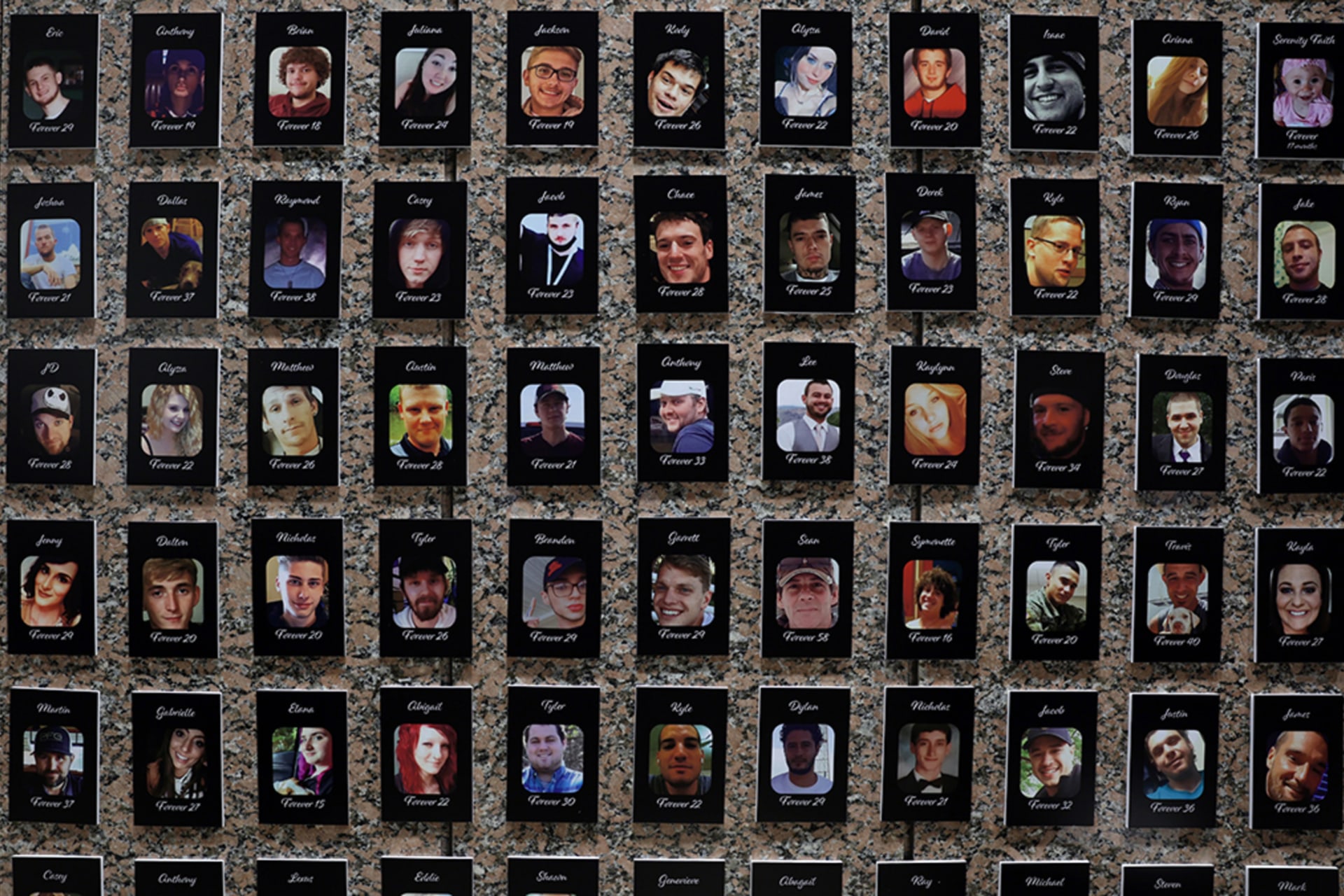
- Backgrounder
Fentanyl and the U.S. Opioid Epidemic
![]()
- Backgrounder
What Does the CDC Do?
![]()
![]() By Thomas J. Bollyky
By Thomas J. Bollyky- Backgrounder
How Vaccines Changed the World
![]()
![]() By Ellora Onion-De
By Ellora Onion-De![]() By Linda Robinson and Noël James
By Linda Robinson and Noël James![]() By Linda Robinson
By Linda Robinson![]() By Linda Robinson
By Linda Robinson![Major Pandemics of the Modern Era cover image]() By Claire Klobucista and Mariel Ferragamo
By Claire Klobucista and Mariel Ferragamo